Is High Pain Tolerance for Individuals With Autism True?
Whether it’s physical, emotional, or mental, everyone suffers from pain at various times and intensities throughout their lives. However, researchers are finding that pain and autism, and how some autistics may have a high pain tolerance, are only now beginning to be understood.
The Urgent Question of Pain Threshold in Autism
 Several studies over the past decade have found that many autistic individuals have a high pain threshold compared to non-autistic people. This means it often takes more intense stimuli to trigger feelings of pain in those with autism. For example, one study applied heat stimuli to boys with and without autism and found that the autistic boys could withstand higher levels of heat before reporting pain.
Several studies over the past decade have found that many autistic individuals have a high pain threshold compared to non-autistic people. This means it often takes more intense stimuli to trigger feelings of pain in those with autism. For example, one study applied heat stimuli to boys with and without autism and found that the autistic boys could withstand higher levels of heat before reporting pain.
While a higher pain threshold has been frequently documented, findings on pain sensitivity and autism and pain tolerance have been more mixed. Some research indicates that autistic individuals’ sensitivity to pain, once it is felt, tends to be the same or even higher than in neurotypical people.
For instance, children with autism rated pain from venipuncture as more intense than non-autistic children. However, other studies have found no differences in pain sensitivity between those with and without autism.
More severe sensory sensitivity, a common feature of autism that includes exaggerated responses to external stimuli, does appear connected to greater pain reactivity. One study discovered that autistic children with heightened sensory over-responsivity and concerns of undefined pain over entire body also had lower pain tolerance. So sensory processing differences in autism seem to play a role in pain experiences.
Expressing Symptoms of Pain and Autism and Possible Chronic Pain Syndrome ICD 10
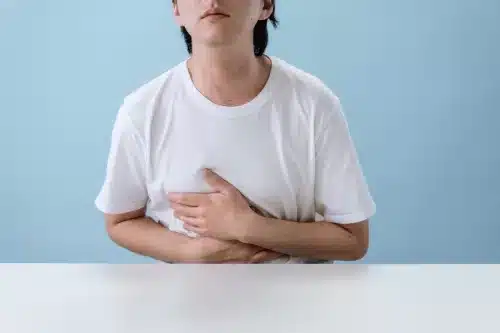
Autistic individuals often communicate and express pain differently than non-autistics.
Many autistic individuals, especially those with limited verbal capacities, have difficulty describing feelings of pain using spoken language. They tend to rely more on nonverbal behaviors to communicate pain, such as facial expressions (grimacing), moaning or crying out, changes in body language (guarding part of the body), or levels of activity (refusal to walk or move around).
Caregivers and medical professionals need additional training to recognize these potential behavioral signs of chronic pain syndrome ICD 10 in autistic patients. Without this understanding, signs of non-targeted pain over entire body may be misinterpreted as externalizing behaviors like aggression or self-injury instead.
Or, pain may go untreated due to lack of self-report when severe verbal communication impairments exist. This further highlights the need to pay greater attention to observed pain behaviors in autism.
Causes and Complications of Unmanaged Pain Due to High Pain Tolerance
Unidentified pain over entire body and poorly managed pain can lead to significant distress and challenging behaviors in autistic individuals.
There are many potential sources of pain and autism, including:
- Gastrointestinal disorders like constipation or acid reflux which commonly co-occur with autism
- Greater vulnerability to inflammation and pain after minor injuries
- Sensory sensitivities leading to headaches or tactile pain
- Menstrual pain and discomfort in autistic girls and women
- An increased rate of chronic health issues like seizures that can cause body pain
- Dental pain and sensitivity during dental exams due to sensory differences
Additionally, the same daily living, medical, and social activities that non-autistic individuals regularly tolerate may result in pain overloads for autistic people. These potential pain triggers include sensory stimuli like loud noises, bright lights, body contact, food textures; medical appointments involving vaccines, blood draws, physical manipulation; or demands for eye contact and social interaction.
When the underlying pain goes untreated in autism, it may result in higher levels of self-injury like skin biting/picking, hitting or banging heads, extreme aggression, or emotional meltdowns as expressions of distress.
Unaddressed pain, often due to being unable to pinpoint the source of pain over entire body, negatively impacts physical and mental health. It can also lead to negative stereotyping and punishment of common autistic behaviors.
Better Understanding of Pain Tolerance and Autism Still Needed
 While research interest in pain and autism has increased in recent years, there are still significant gaps in knowledge. Most studies on pain in autism focus only on children. Yet chronic pain clearly continues from childhood into adulthood for many on the spectrum.
While research interest in pain and autism has increased in recent years, there are still significant gaps in knowledge. Most studies on pain in autism focus only on children. Yet chronic pain clearly continues from childhood into adulthood for many on the spectrum.
Very few studies measure pain during everyday activities or medical procedures – when most pain experiences tend to occur. Little is known about effective pain prevention and pain management strategies tailored specifically to autistic adolescents and adults.
Additionally, nearly all research on pain and autism primarily includes predominantly white, male participants at the high-functioning end of the spectrum. There is a lack of racial, ethnic, gender, and diversity in functioning level representation within study samples.
Since autism manifests differently across identities and abilities, the current research likely does not paint a complete picture. Clearly, more work is needed to understand this connection across the full autism spectrum.
Seeking Solutions: Pain Prevention and Pain Management
While the research on pain tolerance in autism still requires expansion, existing studies do provide some helpful insights on potential pain prevention and management strategies tailored to this population. Here is an overview of some of the main recommendations from health professionals (remember to always consult with your doctor or therapist, as I am not a medical expert):
Pain Prevention
Several methods may help prevent unnecessary pain for autistic individuals when applied proactively:
- Conduct a functional behavior assessment involving caregivers tracking daily activities and pain triggers
- Develop sensory-friendly environments with soft lighting, muted sounds, comfortable spaces to retreat
- Establish and respect pain thresholds for touch, auditory input, and other stimuli
- Prepare for potentially painful events through visual schedules and written narratives
- Teach communication of pain type, location, and intensity through multiple modes
- Encourage regular physical activity and stretching to prevent injury and inflammation
- Implement dietary changes to ease gastrointestinal discomfort
- Explore underlying sources of distress leading to self-injury which communicates pain
Medical Pain Management
Guidance on pharmacologic and therapeutic pain management specific to autism includes:
- Start with non-medication treatment modalities first due to adverse side effect risks
- Administer medications at lower doses with gradual increases to observe reactions
- Attend to gastrointestinal issues first since they exacerbate other pain
- Provide localized pain relief like topical analgesics when possible
- Partner symptom relievers with calming strategies like weighted blankets
- Communicate clearly about procedures and sensations to expect
- Offer multiple modalities including music, imagery, massage, movement
While personalized pain prevention and management plans will differ, these recommendations provide a helpful starting framework. Ongoing support from clinicians, therapists, caregivers and educators is key for implementation success.
Building a Culture of Autism Acceptance and Pain Threshold
Perhaps most critical to improving pain experiences broadly is continuing advocacy to foster a culture and society of autism acceptance, and in particular those with chronic pain syndrome ICD 10. Judgment, discrimination and abuse that autistic individuals face even within healthcare settings unnecessarily exacerbates pain and trauma.
Here is how we can build a community of inclusion:
- Keep expanding research on autism and pain using diverse and representative samples
- Improve autism awareness and sensitivity training for all who support those with disabilities
- Tackle barriers to access for communication aids, mental health services, and integrative pain care
- Develop more sensory-friendly public spaces and destigmatize accommodations
- Celebrate neurodiversity and the contributions of autistic individuals
Progress starts from within through transforming attitudes, language, and action. But change ultimately requires addressing systemic ableism as well. Only with relentless, collaborative effort across personal, professional and policy channels can we achieve equity and justice. The whole of society stands to gain through embracing disability rights as basic human rights.
Pain Management and Pinpointing Source of Pain Over Entire Body
What happens if we fail to prioritize understanding, preventing, and relieving pain in autism? The consequences of inaction are severe.
Unmanaged pain takes a drastic physical and emotional toll on autistic children and adults. Beyond general distress, it can specifically contribute to higher rates of anxiety, depression, sleep issues, and loss of critical life skills.
The immense stress of living with chronic pain syndrome ICD 10 also takes years off one’s health and lifespan.
 In addition, lacking pain relief often leads to an over-reliance on psychiatric medications or mechanical restraints to control externalizing behaviors. Not only does this worsen stigma, but chemical and physical restraints also cause further physical and psychological harm. These desperate measures signify a health system that has neglected its most vulnerable patients.
In addition, lacking pain relief often leads to an over-reliance on psychiatric medications or mechanical restraints to control externalizing behaviors. Not only does this worsen stigma, but chemical and physical restraints also cause further physical and psychological harm. These desperate measures signify a health system that has neglected its most vulnerable patients.
Finally, the trauma of inadequately treated pain has ripple effects across families, caregivers, and communities too. Pain matters – because allowing suffering when relief is possible pains us all. Fostering a culture in which no one has to bear unrecognized and unmanaged pain is ultimately most compassionate for society as a whole.
The ethical imperative here cannot be ignored. Pain care parity through validating lived experiences, amplifying marginalized voices, dismantling barriers, and transforming practices and policies is the only acceptable standard.
With expanded pain research, education, accommodations, alternatives and therapies tailored to autism, we can prevent much unnecessary suffering. Prioritizing progress now will emanate outwards in wide-ranging individual and societal quality of life improvements for generations to come.
In summary, while the correlation of pain and autism remains understudied, it is abundantly clear that proactive and compassionate pain care can no longer be disregarded or delayed. Truly understanding and addressing this connection is foundational to both physical comfort and the realization of neurodiversity rights.
With continued efforts, the gaps in knowledge and practice will close over time. But progress first starts at the grassroots level through families, advocates and organizations elevating consciousness and standards surrounding this issue.
Partnership with ethical health professionals committed to reducing health disparities for people with disabilities will also be integral to systems change.
Fundamentally, pain and humanity cannot be separated – because absence of the former defines the meaning of the latter. When it comes to pain and autism, and especially with chronic pain syndrome ICD 10, confrontation of uncomfortable truths paves the path to freedom and justice. May we have the courage and perseverance to walk it.
Improving Care and Quality of Life As It Relates to Pain Tolerance
Ultimately, better understanding the autism-pain connection has major implications for improving quality of life. It can enable quicker recognition of pain sources by both family members and clinicians.
This allows for faster access to appropriate pain relief treatments, whether that’s medication, therapy, behavioral support, or alternatives. Pain prevention in the form of identifying and controlling sensory input or preparing individuals for potentially painful situations with social narratives and exposure therapy is also key.
Most importantly, comprehension of the pain experiences of autistic individuals leads to more equitable medical care. Autistic children and adults have the right to the same safe and compassionate health care as anyone else.
Making the effort to accurately recognize, communicate about, document, treat, and manage pain in autism is critical – no matter how a patient communicates their pain or distress. Increased awareness and training on this issue for caregivers, educators, and health professionals is an essential step toward more ethical care for people with autism.
As understanding transforms into action, the autism community can demand pain parity and pain relief.
Pain Is Part of Universal Human Experience
While pain itself and learning how to cope with it is part of the universal human experience, it is important to adapt achievable coping skills for managing it. Most everyone has their own coping mechanisms on how they cope with their individualized level pain threshold, and whether a person is neurodiverse or not, healthy coping mechanisms are critical.
Unhealthy coping mechanisms will just make things worse (you can read more about these here).
Understanding the pain and autism experience and how to work through it matters for improving quality of life.
Autism in Adults: Living, Learning, and Overcoming Challenges for a Fulfilled Life
Autism in adults requires additional support and coping skills to achieve independence in today’s world.
Learn more about ways adults can live fulfilled lives and the challenges they face.
- 10 Hot Topics in Autism Research
- Rigid Routine and Why Being Inflexible Can Harm Happiness
- Autism and Independence: 7 Skills That Empower Individuals to Thrive
- Dangers of Social Media Addiction: How To Leave the Screens And Face the Real World
- Autism Volunteer Opportunities: 5 Ways Helping Others Fosters Acceptance
- Top 25 Hurdles Individuals Face Daily on the Spectrum
- Are You An Adult With Autism? Here Are 6 Signs
- Autism vs Asperger’s Syndrome: What You Need to Know
- Autism Disclosure: Is Revealing Your Disorder Helpful or Hurtful?
- Work and Autism: What Employers Should Know About Hiring People with Neurodiversit