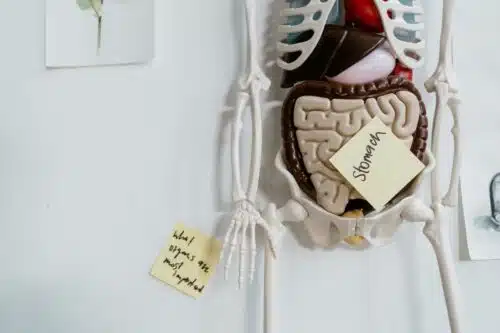
It's a Gut Punch! How to Manage Autistic Gut-Brain Connection
 Many children and adults alike with autism spectrum disorder (ASD) have significant gastrointestinal (GI) difficulties. Problems like constipation, diarrhea, abdominal pain, acid reflux, and food sensitivities are very common, with some reports saying it affects 40-90 percent of individuals with autism.
Many children and adults alike with autism spectrum disorder (ASD) have significant gastrointestinal (GI) difficulties. Problems like constipation, diarrhea, abdominal pain, acid reflux, and food sensitivities are very common, with some reports saying it affects 40-90 percent of individuals with autism.
While ASD and GI issues weren’t initially connected as a co-occurring condition, researchers now recognize an important gut-brain connection that may help explain why autism and GI issues are often linked. Unpacking the gut-brain axis in autism is key to improving symptoms.
If you have struggled with any of the GI issues, It may be time for a gut health check with your doctor. It can be comforting to know it’s not your imagination, or because you are “too picky” with food. Learning more about the gut microbiome, which refers to all the microorganisms living in our digestive system, is important to not only digestive health but also physical and mental health.
The Gut-Brain Axis and What It Means for Autism and GI Issues
The gut-brain axis refers to the communication network that exists between the gastrointestinal system and the central nervous system. As a quick science lesson recap, this axis relies on three main pathways:
- Direct Nerve Connections. The vagus nerve runs from the base of the brain directly to the gastrointestinal tract, heart, and other organs, facilitating what is called a “cross-talk” between the brain and gut.
- Hormone Signaling. Did you know the gut is the largest hormone-producing organ in the body? Hormones produced in the GI tract like serotonin, melatonin, dopamine, and cortisol regulate gastrointestinal function. These hormones also interact with receptors in the brain, which influence our mood, behavior, circadian rhythms, stress responses, and metabolism.
- Immune and Microbial Signaling. The gut microbiome and intestinal immune system have direct and indirect effects on brain function through mechanisms like inflammatory cytokines traveling in the bloodstream and bacterial metabolites crossing the blood-brain barrier.
That’s a lot of science-speak, but simply put, it’s no surprise that things can go wrong, and disruptions anywhere within the gut-brain connection could contribute to symptoms of ASD. Research indicates that autistics often have altered gut microbiota, intestinal inflammation, impaired intestinal barrier integrity, and differences in gut hormone/neurotransmitter levels as compared to neurotypicals.
These gastrointestinal abnormalities could interact with genetic inclinations for ASD to worsen behavioral symptoms.
RELATED: Does Autoimmune Disorder Meaning Connect to the Autism Spectrum?
The Gut-Brain Connection with Microbiome in ASD

In those with ASD, an imbalance between beneficial and pathogenic gut flora (known as dysbiosis) along with a less diverse microbiome profile is common. Several bacterial kinds are overrepresented in autistics, producing neurotoxins and acids that can impair nervous system function. That’s why it can be a punch to the gut!
I’m not a health expert, so autism and GI issues are best made with a healthcare expert, especially when seeking relief or more detailed information. However, many studies indicate that antibiotic use, diet quality, hygiene levels early in life, and genetics are among the influences of microbiome composition. Researchers are studying whether infant gastrointestinal disturbances from these and other factors may trigger inflammation, leaky gut, and abnormal microbial profiles that contribute to developing ASD in genetically vulnerable children.
Leaky Gut Syndrome: Is There A Connection with Autism?
Normally, the intestinal lining acts as a selective barrier that keeps out large molecules like proteins while allowing the absorption of nutrients. In those with ASD, it appears that defects in intestinal barrier integrity often exist, commonly called “leaky gut syndrome.”
Research shows that neurotoxic molecules, undigested food particles, and bacteria can leak from the intestines into the bloodstream when this protective barrier is impaired. Once across the intestinal barrier, these compounds trigger widespread inflammation and autoimmune reactions that appear to worsen behavioral symptoms of ASD.
Not only does a leaky gut allow the access of toxins, but dysbiosis and intestinal inflammation themselves increase intestinal penetrability further, resulting in a vicious cycle. Even subtle intestinal inflammation is very common in ASD, which studies say contributes to nervous system disturbances.
The Second Brain and Its Effects on ASD
Serotonin produced in the gut plays a key role in intestinal motility, secretion, and signaling within the enteric nervous system (sometimes called the “second brain”). Serotonin also communicates with the central nervous system. In autistics, altered serotonin levels are common.
Since about 90% of the body’s serotonin is actually produced in the intestines, GI factors can play a major role in the serotonergic abnormalities seen in autism spectrum disorders. Dysregulation of serotonin from the gut likely affects both bowel function and behavioral issues in ASD. At least that’s the theory, according to numerous studies.
LEARN MORE: What Are Top 25 Autism Spectrum Disorder Symptoms?
Unhealthy Diets, Food Sensitivities, and GI Symptoms
Many autistics have severe selective eating habits, food sensitivities, and gastrointestinal symptoms like chronic constipation that add to distress and behavior issues. Diets high in refined carbohydrates and processed foods combined with low nutrient intake from fruits, vegetables, and quality proteins often lead to dysbiosis and impaired gut function.
In fact, some studies show that the severity of GI symptoms correlates with the severity of autistic behaviors. This could be due to unhealthy diets and GI issues.
For children and adults alike with ASD, a comprehensive medical and nutritional approach focused on a gut health check is a critical piece of the treatment puzzle. Strategies like removing allergenic/inflammatory foods from the diet, adding digestive enzymes and probiotics, combating bacterial/fungal overgrowth, and repairing intestinal permeability help reduce GI and behavioral symptoms for many.
The Chicken or the Egg – Origins of Autism and GI Issues
This concept of a “gut-brain axis” may help explain why autism often develops suddenly between ages 12-24 months following an illness, infection, or period of severe GI symptoms. The right triggers at key developmental windows could set off a cascade toward autism in high-risk kids. But, again, I’m not the expert and am just reporting studies.
It also seems clear that not all cases of ASD follow this pattern. In other subsets of children and adults with autism, it appears that a primary genetic/neurologic trigger leads to the development of GI problems secondary to behavioral issues and restricted diets associated with ASD. Clearly, more research into distinct autism phenotypes and their origins is needed.
While researchers don’t yet fully understand the origins of ASD, experts do know that GI interventions often lead to improvements in both bowel symptoms as well as behavior and cognition.
By addressing “leaky gut” and related issues through special diets, supplements, medications, and other treatment options, many patients see substantial benefits. This has profound implications for treatment and prevention.
RELATED: Is High Pain Tolerance for Individuals With Autism True?
The Gut-Brain Axis and Autism: Emerging Treatment Options
As health experts learn more about connections between gastrointestinal health and autism spectrum disorder, new dietary, supplemental, and medication treatment options are emerging that target the gut-brain axis.
If you or your child have GI issues, don’t just suffer with them. Seek medical support and assistance. Treatment could greatly improve quality of life, and that’s what anyone wants. Here are gut health check treatment options often considered:
Elimination Diets
Removing commonly allergenic foods like gluten, casein, soy, corn, eggs, and dairy may improve GI symptoms, reduce inflammation, and improve behavior in children and adults with ASD. Following an elimination diet under the guidance of a nutrition professional ensures nutritional adequacy.
Reintroducing foods one at a time can help identify personal food intolerances.
Probiotics and Prebiotics
Supplementing with strains of beneficial bacteria shows promise for supporting a healthy, diverse gut microbiome, reducing gastrointestinal issues and problem behaviors in ASD. Prebiotic fibers that feed good gut flora are also helpful. Emerging microbiome analysis could allow for personalized probiotic formulas.
Gut-Brain Peptides
Supplements could help support the regulation of neurochemistry, anxiety, sleep, and GI motility issues in ASD by activating receptors in the enteric nervous system. L-theanine, magnesium, and flaxseed oil could also have gut-brain benefits.
Prescription Medications
In more severe cases of autism and GI issues, ASD specialists may prescribe medications like antifungals to clear Candida overgrowth, gut-directed antibiotics for bacterial imbalance, motility agents for constipation, or anti-inflammatories for inflammatory bowel conditions.
Gut Health Check: The Bottom Line

However, considering the gut-brain connection in autism appears critically important for better understanding this mysterious disorder. The gastrointestinal system may offer unique treatment targets and prevention strategies that help individuals with ASD find greater health, learning, and quality of life.
Hopefully, more research exploring individual differences in GI function could pave the way for personalized medicine breakthroughs.
Additional Challenges Individuals with Autism Face
Learn more about other issues that autistics face:
- Being Real Without Offending Othersis an Autistic Challenge
- Autism and Organization: The Secret to Finding Calm in the Chaos
- Helpful Self-Regulation Tipsfor Keeping Calm and Carrying On
- New Research Reveals Autism Mental Health Linked to These Disorders
- Is Autism a Disability? Surprising Reasons for the Debate
- Social Justice Issues: Why Disability Rights Matter for Autistics
- Break Free: 10 Tips to Take A Risk and Escape Your Comfort Zone
- Autism and Holidays: Why Special Occasions Can Be Challenging
- 6 Fascinating Facts About Autism You Probably Didn’t Know
- 8 Popular Ways to Manage and Master Autistic Social Awkwardness
- Autism and Poor Hygiene: The Smelly Truth to Overcome
- Breaking Down Barriers that Challenge Autism and Friendships
- Anxiety and Autism: 5 Powerful Strategies to Conquer Emotions
- 6 Ways to Tackle Autism Fireworks Anxiety and Sensory Overload
- Autism Clothing for Sensitive Skin Can Enhance Quality of Life
- Autism After High School: Is College the Next Step?
- Climate Change and Its Alarming Impact on Autism Emotion