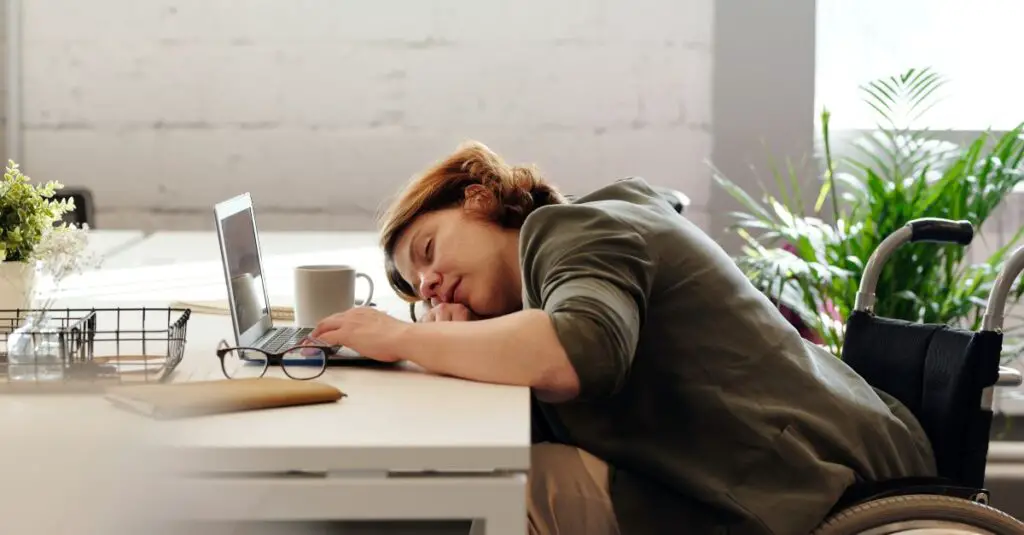
Autism and Sleep: 4 Ways That Destroy Restful Slumber
Sleep issues are very common among individuals with autism spectrum disorder (ASD). In fact, some studies show that up to 80% of children on the spectrum experience some type of autistic sleep disturbance, compared to 25-40% of typical children. The struggle unfortunately continues into adulthood as well (I speak from experience).
The most common autism sleep disorders include insomnia, sleep apnea, restless leg syndrome, and circadian rhythm disorders. The lack of quality autistic sleep can have significant impacts on daytime functioning and affect overall quality of life as a result.
 The connection between autism and sleep disorders has multifaceted reasons. Many individuals with autism have heightened sensitivities to sensory stimuli, making it challenging for them to wind down at bedtime.
The connection between autism and sleep disorders has multifaceted reasons. Many individuals with autism have heightened sensitivities to sensory stimuli, making it challenging for them to wind down at bedtime.
They may also have difficulty regulating their internal body clock or exhibit irregular sleeping patterns due to neurological factors associated with autism.
By understanding the connections between autism and insomnia and other autism sleep disorders, as well as effective treatment strategies, falling asleep and staying asleep can greatly improve a person’s mental and physical health.
Here are key challenges that cause autistic sleep problems.
4 Top Reasons for Autistic Sleep Challenges
Insomnia
Autism and insomnia, which is defined as difficulty falling or staying asleep, is perhaps the most prevalent sleep disorder among people on the spectrum. Many factors can contribute to the lack of autistic sleep:
- Anxiety – Many people with ASD experience anxiety, worrying obsessively about upcoming events/activities. This racing mind can make it very difficult to unwind at night.
- Sensory sensitivities – Sensitivities to sound, light, temperature, and textures may cause discomfort that prevents sleep. Some may also have tinnitus or other sensory issues only noticeable when trying to sleep.
- Gastrointestinal issues – Constipation, acid reflux, and other GI problems can disrupt sleep. There is a strong connection between autism and GI and/or autoimmune issues.
- Melatonin dysregulation – Melatonin is the hormone that controls sleep/wake cycles. Those with ASD tend to have lower levels of melatonin as well as atypical production patterns.
- Hyperarousal – Many exhibit heightened sensory sensitivity and cognitive hyperactivity, making it difficult to “switch off” at night.
- Genetic mutations – Research has linked insomnia in autism to mutations in genes that regulate melatonin and serotonin.
The lack of sleep from autism and insomnia can then lead to significant daytime problems for those with ASD including:
- Behavior issues – Irritability, tantrums, noncompliance, and aggression may increase with poor sleep.
- Attention/learning difficulties – Insomnia impairs focus, motivation, memory, and ability to process information.
- Mood swings – Inadequate sleep often leads to symptoms of anxiety, depression, and overall emotional volatility.
- Health problems – Lack of sleep strains the immune system and impacts cardiovascular, metabolic, and mental health.
Sleep Apnea
Pauses or a decrease in breathing characterize sleep apnea, one of the primary autism sleep disorders. This prevents people from reaching deep, restorative stages of sleep. Autistic sleep apnea may be related to:
- Differences in mouth/airway anatomy – Some have altered bone structure or low muscle tone that can cause airway obstruction.
- Enlarged tonsils/adenoids – Common in childhood, enlarged tonsils narrow the airway.
- Obesity – Excess weight and fat deposits increase the risk of airway collapse.
- Sedative medications – Some medications used for managing anxiety, OCD, or seizures can overly relax muscles.
Common symptoms of sleep apnea include:
- Loud snoring
- Restless sleep with frequent waking
- Excessive daytime sleepiness
- Morning headaches
- Bedwetting in children
Studies show sleep apnea has been associated with the following behavioral issues in autism:
- Aggression and self-injury
- Hyperactivity and inattention
- Oppositional and non-compliant behavior
- Impulsivity
- Irritability and tantrums or meltdowns
Proper diagnosis and management of sleep apnea is critical for those with ASD. Treatment may involve surgery, dental devices, CPAP machines, weight loss, or switching medications. Ongoing screening and monitoring is key, as sleep apnea can develop later even if not present as a child.
Restless Leg Syndrome
Restless leg syndrome (RLS) is both a sensory and motor disorder.
It causes uncomfortable sensations in the legs along with an irresistible urge to move them. Symptoms are most prominent during periods of inactivity and at night. This prevents quality sleep from occurring. Though not extensively studied, there does appear to be a correlation between RLS and autistic sleep.
Potential contributing factors between autism and sleep and RLS include:
- Iron deficiency – Low iron disrupts dopamine activity, exacerbating RLS. Iron deficiency is common in autism.
- Dopamine dysfunction – Dopamine is a brain chemical crucial for controlling movement. Disrupted dopamine processing may play a role.
- Genetics – Studies have identified shared gene variants between RLS and ASD, suggesting a genetic predisposition.
Managing symptoms of RLS can be very beneficial for improving sleep quality and associated daytime issues such as irritability, poor focus, and behavioral outbursts. Treatment approaches include iron supplementation, dopamine agonist medications, vibration therapy, warm baths, massage, and lifestyle changes.
Circadian Rhythm Disorders
Our circadian rhythms function as an internal biological clock that guides the cycles of wakefulness and sleep. Circadian rhythm disorders occur when this natural rhythm becomes disrupted.
Experts say they are common among those with autism due to various factors:
- Melatonin irregularities – Many have low/atypical melatonin levels, which impairs sleep cycle regulation.
- Inflexible routines – Difficulty shifting routines to accommodate earlier/later sleep schedules.
- Lack of exercise – Inactivity suppresses sleep drive and melatonin secretion. Many with autism have limited exercise.
- Genetic mutations – Research links circadian disruption in ASD to mutations in clock genes that control rhythm timing.
Some examples of circadian rhythm disorders include:
- Delayed Sleep Phase Disorder – Falling asleep/waking later than desired due to a delayed circadian clock.
- Irregular Sleep-Wake Rhythm – Inconsistent and poorly consolidated sleep and wake times.
- Non-24-Hour Sleep-Wake Disorder – Circadian rhythm delayed by over an hour daily resulting in later bedtimes.
These circadian disruptions conflict with required school/work schedules and lead to daytime sleepiness. For teens and adults, this autistic sleep issue exacerbates problems with attention, cognition, behavior, and mood already common in ASD.
Treatment Considerations To Help with Autism Sleep Disorders
While sleep issues can certainly be challenging for those with ASD, various treatment strategies exist. As always, be sure to discuss autism and sleep concerns with a medical professional to decide together what could be the best courses of treatment.
Potential tips to help with autism and sleep can include:
- Maintain a regular sleep schedule with consistent bedtime and wake-up times, even on weekends.
- Optimize the sleep environment – comfortable, cool, dark, quiet, and gadget-free. Use white noise if needed to block disruptive sounds.
- Address medical issues that may interfere with sleep such as gastrointestinal disorders, sleep apnea, restless leg syndrome, etc.
- Manage anxiety and sensory sensitivities by establishing relaxing pre-bedtime routines.
- Consider melatonin supplementation under the guidance of a doctor. Melatonin helps regulate circadian rhythm. Most benefit from doses 30 minutes before bedtime.
- Eliminate caffeine, large evening meals, and vigorous exercise within 2-3 hours of bedtime.
- Use visual schedules and social stories to teach healthy sleep hygiene habits. Make schedules very concrete and specific.
- For teens/adults with delayed sleep phase, consider gradually shifting bedtime earlier. Bright light therapy in the morning can also help reset circadian rhythm.
- Seek support services as needed such as a pediatric sleep specialist or clinic for comprehensive evaluation and treatment.
- In severe cases, medications to address sleep issues may be prescribed but should be used cautiously and monitored closely under a doctor’s care.
The Role of Parents in Helping with Autistic Sleep Problems
 Parents play a critical role in helping their autistic children develop healthy sleep habits. However, this can be very challenging when children have autistic sleep issues.
Parents play a critical role in helping their autistic children develop healthy sleep habits. However, this can be very challenging when children have autistic sleep issues.
Some helpful tips for parents include:
- Closely observe your child’s sleep patterns to identify autism and insomnia issues. Note bedtime/wake time, number and duration of night waking, snoring, restlessness, daytime sleepiness, etc. Share this information with your pediatrician.
- Work as a team with your child’s doctor, therapists, and teachers to implement consistent sleep strategies across all settings. This continuity is vital.
- Try to reschedule appointments and meetings to accommodate sleep schedules whenever possible. Protect daytime nap/quiet times.
- Make sleep a family priority above other activities. Don’t overlook the importance of healthy sleep.
- Be patient – it can take time to resolve sleep problems. Stick with a consistent bedtime routine.
- Avoid sleep crutches that become bad habits like letting the child sleep in your bed.
- Limit stimulating electronic media usage for 1-2 hours before bedtime.
- Try calming activities before bed like warm baths, gentle massage, soft music.
- Use social stories and visual aids to teach the child sleep skills step-by-step.
Seeking Support for Autism and Sleep Concerns
If your child’s sleep problems persist despite your best efforts, don’t hesitate to seek professional support. Many resources exist:
- Your pediatrician can check for underlying physical causes like sleep apnea or GI issues. Ask for a referral to a sleep specialist if needed.
- A child psychologist can help with anxiety management, bedtime fears, and behavior modification strategies.
- Occupational therapists address sensory aspects that may disrupt sleep.
- Speech therapists teach relaxation techniques and social skills for bedtime.
- Special education teachers can modify daytime schedules if lack of sleep impacts school performance.
- Sleep clinics offer comprehensive evaluation and treatment. Some clinics cater specifically to the needs of children with special needs.
- Support groups connect parents facing similar sleep challenges. Feedback from other parents can be very helpful.
- There are also great books, podcasts, and blogs full of tips for improving sleep in autism.
Don’t lose hope! Keep working closely with your child’s support team to find the best solutions.
Autism Sleep Disorders Tips for Adults
While a lot of focus goes to improving children’s sleep, adults on the spectrum struggle with sleep as well. Those with autism and insomnia, sleep apnea, and other disorders may benefit from these tips:
- Maintain a structured pre-bed routine to transition and unwind.
- Limit stimulating media use before bedtime.
- Avoid caffeine, alcohol, heavy meals, and exercise within 2-3 hours of bedtime.
- Make your bedroom as comfortable and sensory-friendly as possible. Use blackout curtains or a sleep mask.
- Ask your doctor about melatonin supplements to regulate the sleep cycle. Take 30 minutes before bedtime.
- See your doctor right away if symptoms like snoring or constant fatigue occur. Don’t ignore potential sleep apnea.
- If anxiety keeps you up, try relaxation techniques like deep breathing, meditation, and massage.
- Keep a journal by your bed to jot down thoughts and worries at night.
- Maintain a regular sleep-wake schedule, even on weekends. Gradually shift if needing to adjust timing.
- Join an autism support group and exchange tips with others experiencing similar sleep struggles.
- See a sleep specialist for help if sleep problems persist despite lifestyle changes.

Prioritizing sleep hygiene takes work but pays off by improving mental and physical health. Don’t resign yourself to sleeplessness – take active steps to restore healthy sleep patterns.
Sleep is a basic need everyone has; you just can’t function at your best without getting good sleep. Being well rested is vital to live a good life, as it’s hard to live your best life if you’re always groggy. So don’t underestimate the value the quality of a good night’s rest and do everything you can to ensure you sleep well.
The impact of autism and sleep problems should not be underestimated. Promoting healthy sleep provides far-reaching benefits for daytime learning, behavior, health, and quality of life for autistic individuals. A comprehensive, individualized approach that identifies and targets the root causes of autism sleep disorders for each person can pave the way for better days ahead.
By working on these tips, you’ll see there are some sound ways to get a good night’s sleep that go beyond simply counting sheep!
Additional Challenges Individuals with Autism Face
Learn more about other issues that autistics face:
- New Research Reveals Autism Mental Health Linked to These Disorders
- Neurodiversity in the Workplace: Finding the Right Job
- Is Autism a Disability? Surprising Reasons for the Debate
- Autism and Holidays: Why Special Occasions Can Be Challenging
- 6 Fascinating Facts About Autism You Probably Didn’t Know
- 8 Popular Ways to Manage and Master Autistic Social Awkwardness
- Autism and Poor Hygiene: The Smelly Truth to Overcome
- Breaking Down Barriers that Challenge Autism and Friendships
- Growing Up Autistic: How I Overcame Challenges and Now Thrive
- 6 Ways to Tackle Autism Fireworks Anxiety and Sensory Overload
- Autism Family Support: 5 Ways to Achieve A Happy Household